What is a Meniscus?
In each knee there are two meniscal cartilages a medial (inside) and lateral (outside) meniscus. The role of the meniscus is to act as a shock absorber between the femur (thigh bone) and tibia (leg bone). The meniscus is commonly referred to as a cartilage, but should not to be confused with articular cartilage (another form of cartilage that lines the bone).
The meniscal cartilages move as the knee bends or straightens - Unfortunately sometimes the meniscus can get pinched between the two bones and will tear, or as the person ages the meniscus starts to degenerate and will tear.
Age Groups
Acute or traumatic tears of the meniscal cartilage occur in predominantly younger people through sports injuries. They do commonly occur with other injuries to the knee such as cruciate or collateral ligament injuries as well.
The other age group that meniscal cartilage tears occur in are those between the ages of 35 and 60. These tears are generally atraumatic and represent a degenerative (wear and tear process) of the meniscus that eventually leads to a tear.
Signs
Effusion: This is swelling within the knee joint itself and is detected by moving fluid around the knee
Quadriceps muscle wasting: If the knee is not being used normally the quadriceps muscle will start to lose its bulk.
Gait: How a person walks may be affected by a meniscal tear
Joint line tenderness: One of the best tests for determining if there is a meniscal tear. The patient will be tender on either joint line. The reason for this is that this is where the meniscus is located.
Meniscal provocation tests: Nigel will perform these tests to determine if a tear is present. In combination with joint line tenderness and an effusion it is highly likely that a meniscus tear is present.
Range of movement: If the knee is truly locked, it will be bent and no amount of movement will unlock the knee. This has to be dealt with on an urgent basis, to help relieve pain, but also to repair or remove the part of the meniscus that is torn.
Imaging - MRI Scan
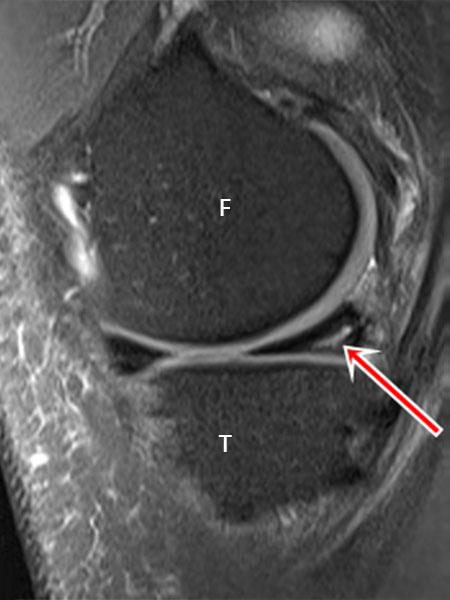
A MRI scan helps if Nigel is unsure of the diagnosis or if he suspects there are other structures damaged in the knee. What the scan above shows is a tear in the posterior horn of the medial meniscus (most common place for a tear). The arrow demonstrates the tear (it is the white line seen in the black triangle. F=Femur, T=Tibia.
Options for Treatment
Surgery is not recommended for all patients. If your knee has no swelling, no pain on activities, is not catching or getting stuck, and you have a full range of movement then surgery in my opinion is not necessary. It does not mean that you will not require surgery in the future but it does mean that you do not require surgery now. I will generally give your knee 8 weeks to settle down. If it has not done so by 8 weeks then it is probably not going to settle and I would recommend surgery at that time.
If your knee has swelling, with pain, a limited range of movement aand my examination, along with MRI shows a tear then I may recommend arthroscopy (key-hole surgery) of the knee.
If I am unsure of whether there is a tear of the meniscus or if I think there is other damage in the knee, I will get a MRI scan of the knee first, then discuss the findings of the MRI scan before deciding whether surgical intervention is necessary.
Surgery Options
Arthroscopy
Arthroscopy is a surgical technique that can be used in treating Meniscus Injuries.
Meniscectomy
- Total Meniscectomy is removal of the entire meniscus from the knee. This is uncommon today
- Partial meniscectomy is where only the torn part of the meniscus is removed and the rest of the meniscus is left
- Meniscal repair is where the meniscus is repaired with sutures. This is preferable in a small number of cases. Nigel will discuss with you if this is suitable for your torn meniscus.



